Bird Flu: Another Pandemic?
The Dirt
In the past three months, H5N1, otherwise known as Avian Influenza or Bird Flu has transmitted from birds to dairy cows. This virus transfer has caused alarm and confusion, spurring misinformation about the trust in our food system. In this post, we're not jumping to conclusions on H5N1 - we're digging into the latest research and discussing its implications.
Global Food
Bird Flu: Another Pandemic?
The Dirt
In the past three months, H5N1, otherwise known as Avian Influenza or Bird Flu has transmitted from birds to dairy cows. This virus transfer has caused alarm and confusion, spurring misinformation about the trust in our food system. In this post, we're not jumping to conclusions on H5N1 - we're digging into the latest research and discussing its implications.
As of this writing, in 2024 only three dairy farm workers have caught this virus. However, the concern is that it has been transmitted to humans from dairy cows and could potentially be transmitted from human to human. As of today, there is no evidence that it has transferred from person to person.
We spoke to Dr. Kenneth Odde, veterinarian, beef cattle operator, and former Professor at Kansas State University. who stated:
“The risk of a pandemic is very low. It will never be zero, but with everything I understand, it is low”.
Let’s start at the beginning…
In 1996, H5N1 was first detected in domestic waterfowl in southern China. It then spread to farmed poultry. A small number of people caught the virus who worked in very close proximity to their birds: touching, feeding, and cleaning their cages.
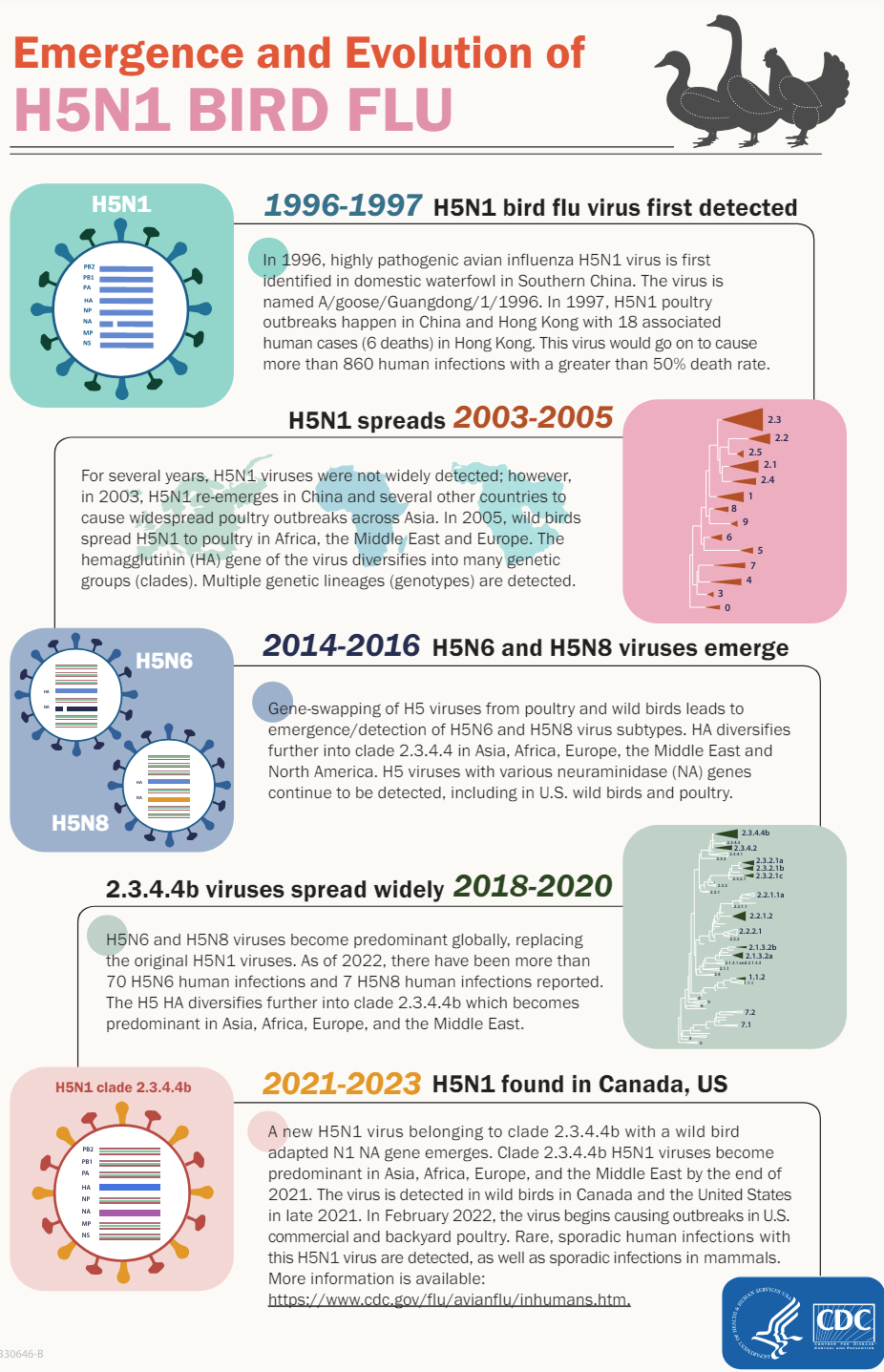 Over time, 860 people were identified with the virus and there was a 50% death rate. Governments and companies around the world began preparing for a pandemic.
Over time, 860 people were identified with the virus and there was a 50% death rate. Governments and companies around the world began preparing for a pandemic.
However, the virus stayed mainly in Asia and was fairly dormant until 2003 when it affected widespread poultry.
Wild birds then spread H5N1 to Africa, the Middle East, and Europe. The H5N1 virus continues to evolve and has become well-adapted to spread efficiently among wild birds and poultry. In 2021, new variants of the H5N1 virus were spread by wild birds in the U.S. and Canada.
Because wild birds easily spread it, commercial poultry flocks have been affected across the country. H5N1 is highly pathogenic (deadly) to birds, and when one bird gets it, the entire flock is at risk and is culled. While not as prevalent, this has affected backyard poultry operations as well.
In March of 2023, we wrote about how H5N1 has affected mammals all over the country: sea lions, minks, otters, foxes, and even bears. At the time, the CDC said that these bird flu viruses didn’t have the ability to bind to the human respiratory system.
H5N1 in the news today
The concern today is that the virus has spread from wild birds to dairy cows.
Unlike birds, dairy cows are only mildly sick for about 7 – 10 days. Once a bird infects one cow, the virus spreads from cow to cow by contact with either through their respiratory system and/or unpasteurized milk droplets. For instance, workers could unknowingly spread the unpasteurized milk among cows. Or the milking equipment and transport vehicles could carry droplets of infected milk.
So far, in 2024, there have been three human cases with dairy farm workers. As a result, two individuals just had a minor eye infection which was easily resolved with antiviral medicine. The third did get flu-like symptoms and recovered with Tamiflu.
Because this is not widely tested among people, it is hard to know if more farm workers have had flu-like symptoms that would be attributed to H5N1. Symptoms can appear to be a mild cold or flu. Neither of these would make one think to go to a Dr. for an Avian Influenza test.
But there are a lot of unanswered questions. Why do some birds and animals react differently to the same virus? For instance, why do mammals such as sea lions, otters, and bears die from H5N1, and dairy cows can recover?
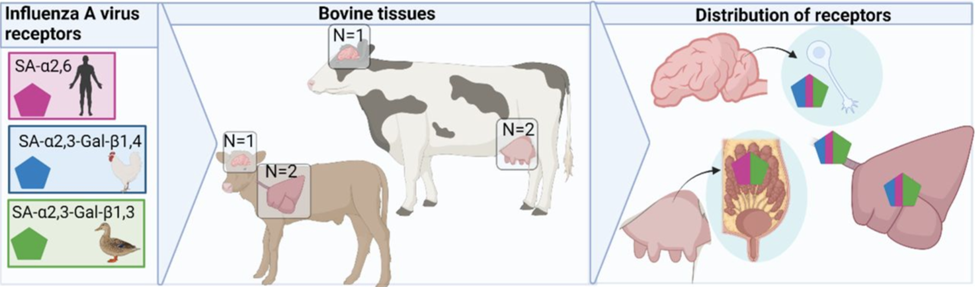
Dr. Odde explained that there is a difference in how a species receives the virus. Recent research shows that the receptor influences influenza symptoms within poultry or mammals. Receptors are proteins within the body that let a virus enter the cell. He also emphasized that many studies are being conducted right now to understand how the virus passes between and among species.
As you know, the best way to stay healthy is to wash your hands before touching your nose, eyes, and mouth. This is because humans have receptors in our respiratory system and you can get sick when a virus touches our respiratory system. The same principle applies to H5N1. Dr. Odde also reminded us that we have had much exposure to the flu over the decades so that humans will have some resistance to H5N1.
Chickens seem to be more susceptible as they receive the virus through their trachea in their respiratory system. Ducks do not have the same mortality rate and early studies show that the virus enters the cells through a different receptor.
Dairy cows receive the virus in their mammary glands as well as their respiratory system. This is not common and is a cause for concern for the replication of H5N1. As of this writing, H5N1 has been detected in 12 states and 92 herds.
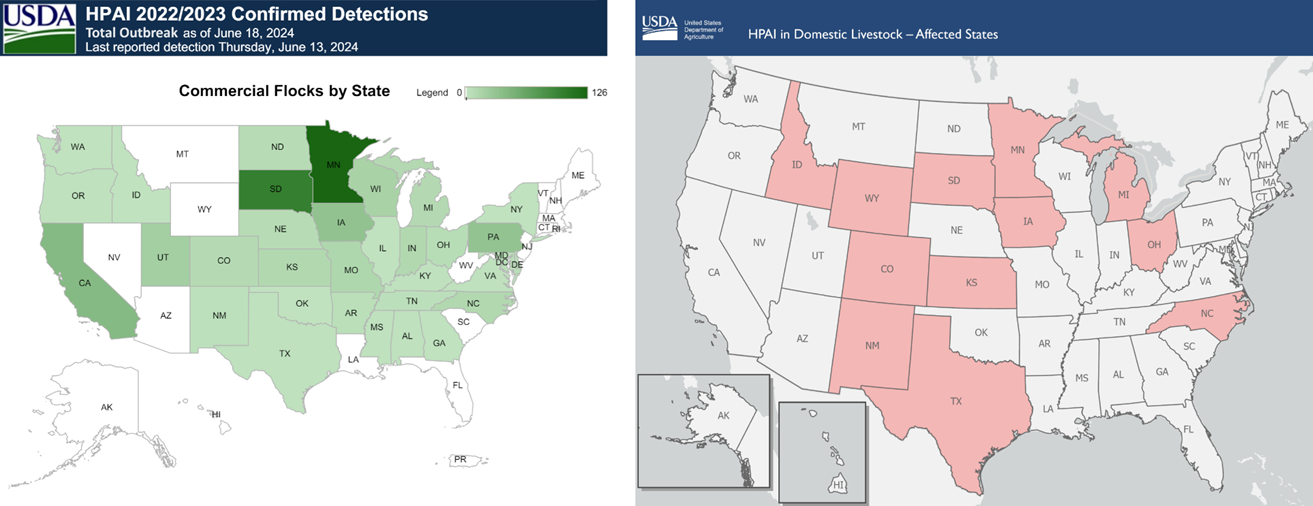
Sources for USDA data: Commercial flock detections by state; HPAI in domestic livestock
Is our food safe?
Yes!
There is no need to be worried about the milk from the grocery store. The pasteurization process kills all bacteria and viruses. 99% of all dairy farmers who sell milk for public consumption follow the Pasteurized Milk Ordinance and participate in the Grade “A” milk program.
To be sure this applied with H5N1, the FDA took milk samples from retail locations in 17 states representing 132 milk processing locations in 38 states. H5N1 was not present in any of the samples.
Raw milk poses the danger. Some people think that raw milk has more amino acids, vitamins, and minerals and is a better choice for your immune system. That is not necessarily true as homogenization and pasteurization doesn’t kill the benefits of milk, it only kills the pathogens. Drinking raw milk, can lead to food-borne illnesses, including H5N1 if it is present.
Eggs are safe to eat. Because Avian Influenza rapidly affects a poultry flock, the eggs are not sold on the market. However, like milk, if you cook your eggs properly and do not eat a raw egg, the chance of getting H5N1 is reduced even further.

The USDA is confident that the meat supply is safe. Ground beef samples were collected in states where dairy herds have tested positive for H5N1 and no virus particles were present. Cooking burgers to 120, 145, and 160 degrees Fahrenheit ensures further safety.
The USDA also reminds us that safe poultry follows the same guidelines as all meats. If handled and cooked properly, poultry is safe. As a reminder, CLEAN, SEPARATE, COOK, and CHILL are good guidelines for safe food in your kitchen.
Backyard poultry can also be affected by wild birds. If one of your chickens dies unexpectedly, you should get it tested by your veterinarian. Also, wash your hands after handling your chickens and the eggs. And of course, cook your eggs properly.
How is the government maintaining food safety with H5N1?
Three government agencies are focused on solving Avian Influenza:
- The FDA is testing milk, poultry, and beef to ensure it is safe
- The CDC protects public health, actively monitors the situation, and provides updates
- The USDA is overseeing dairy producers and proper herd management
In particular, the USDA has added $824 million, to the $1.3 million designed for poultry, to give dairy producers the ability to monitor the health of their herds with continual testing to understand the scope of H5N1.
Once a farm has been disease-free for three weeks, they can then move their animals to different farms. This will also give the USDA an understanding of how producers with affected herds can show elimination of the virus.
Going beyond just the USDA, we spoke to Dr. Lisa Koonin, Founder and Principal at Health Preparedness Partners which helps businesses, nonprofits and governments plan for future health emergencies. She is also an Adjunct Professor at Indiana University. During her 30+ year career at the CDC, she worked as a Director and Deputy Director of the agency’s Influenza Coordination Unit.
“For every human infection that occurs, we are that much closer to a pandemic because the virus adapts to a human and can spread to other people or to animals and then to people.”
– Dr. Lisa Koonin
Dr. Koonin identified six suggestions for these agencies to prevent H5N1 from a widespread dairy pandemic.
- Increase virus surveillance. Test dairy workers and cows in both affected and non-affected areas
- Increase wastewater testing. Sewers that test positive for viruses and bacteria can give us an early warning if it is in the community.
- Promote worker safety. Make sure that farm workers have protective equipment available.
- Communicate with farmers and producers. It is important that those who operate dairy production and poultry farms know how to test, prevent and detect outbreaks.
- Stay away from raw milk. Raw milk can contain a number of disease-causing viruses and bacteria, including H5N1.
- Communicate with the public. It is important that current information about what is known about the outbreak is provided to the public in a timely way. People should avoid close, long, or unprotected exposures to sick or dead animals, including wild birds, poultry, other domesticated birds, and other wild or domesticated animals (including cows).
- Prepare vaccines. It is not known if this virus will spread and become a widespread outbreak. However, several countries are developing and procuring vaccines just in case they are needed.
The Bottom Line
Your food is safe if you handle and cook it properly. Testing conducted thus far has not found changes in the virus that would make it more transmissible to humans. While another pandemic caused by this outbreak is unlikely, we still have many questions about the virus and how it affects birds and mammals. Dr. Koonin reminds us that vigilance is required and the facts might change with additional studies and new information.